|
For soldiers suffering from traumatic brain injury and the psychological effects of war, an art therapy program could provide relief.
The skull’s left corner is gone, leaving a jagged, diagonal edge drenched in red. The eyes are black and frantic. All of it resembles the Iraqi man who, in his final minute alive, stared up at Maj. Jeff Hall. For five years, that face tortured Hall, once a sharp Army leader later shoved to his own ragged edge. Not long ago, a woman handed Hall a blank mask, brushes and paints. She asked him to see what may emerge on the surface. “That image, seared into my mind, began leaking out of me,” said Hall, one of hundreds of active-duty troops who have created masks as part of an art therapy program at Walter Reed National Military Medical Center. “I almost needed to regurgitate it. To be honest, it helped me let it go.” Many more masks, some resembling Hall’s violent creation, some depicting abstract demons, adorn walls at the National Intrepid Center of Excellence (NICOE) on the Walter Reed campus. They reveal scars once carried and cloaked inside the minds of men and women back from war — troops diagnosed with mild brain injuries and secondary psychological issues, including post-combat stress. Hall, 43, who titled his mask “The Shock of Death,” served a pair of year-long tours in Iraq spanning 2003 to 2005. Ultimately haunted by violent events he saw and survived in Iraq, including the loss of friends, Hall eventually contemplated suicide and became more isolated. His commander noticed Hall's behavioral changes and guided him into counseling in 2008. Two years later, Hall was invited to seek treatment for a traumatic brain injury at then-new NICOE, a Department of Defense facility offering research, education and treatment focused on TBIs and psychological health. When service members initially enter the art-therapy studio, their faces often are blank and unyielding, hiding unwelcome war souvenirs within — the mental cargo they’ve lugged home but can’t shake. On their masks, they expose that secret turmoil: vulnerabilities, anger, grief or, often, fragmented identities. “It’s intense. They get really invested in this. It becomes very meaningful for them,” said Melissa Walker, an art therapist who coordinates the masks program. Participants at NICOE must be active-duty troops who are dealing with a combination of TBI and psychological health concerns. Typically, they are referred by their primary health care provider or their commander. A designated team at NICOE determines which service members are most appropriate to receive treatment there. Attendees participate for four weeks. Art therapy is just one of the tools offered and the service members usually make one mask — done during their first week at the center. “I tell them: ‘Don’t worry about the finished product; worry about what you are symbolizing in the mask.’ That makes it more powerful to them. It gives them a way to express to us, visually, what they’re going through,” Walker said. “It’s a little less intimidating then handing them a blank piece of paper.” Art therapy has become a staple in the treatment of a wide array of traumas, from child abuse to PTSD. Making art can help people unlock dark emotions or memories that they can't yet vocalize, pulling those buried anxieties from their subconscious and placing them onto a canvass or into a lump of clay, said Donna Betts, a professor in the art therapy program at George Washington University. As a patients' pieces are taking shape, art therapists help them talk about what they believe they are trying to express in their creations, Betts said. "It's especially effective in the treatment of trauma in service members. When trauma is experienced, it tends to be stored in the nonverbal part of the brain," Betts said. "This is why so many of them can't even put into words what they've been through. Art therapy helps them retell their story through art. It translate that trauma from the nonverbal part of the brain to the verbal part so they can start dealing with it. "They then become more aware of the trauma. This is where that healing starts to take place." After the paint is dabbed and stroked at NICOE, many of those papier-mache masks offer chilling accounts of what it is like to live inside the minds of combat veterans. One brown face with the mouth agape and with bloodshot eyes upturned is squeezed by a metal clamp that reads “TBI” on the left and “PTSD” on the right. Another mask is coated by small chunks of amber bark — two tiny holes remain for eyes — symbolizing the outer camouflage the maker felt is necessary to blend back into the civilian world. Some masks show mouths locked or sewn closed, whispering of an inability to speak of what they’ve witnessed. Many are divided down the middle — for example, one displays part of an American flag on the left and a skull on the right. “There is a split sense of self. They feel like they’re one person when they’re deployed and one person when they return home,” Walker said. “Or, they do a really strong, warrior exterior with a vulnerable inside but they don’t feel like they can express that.” The troops who come to NICOE for therapy can take their masks home. But many purposely leave them to hang from the walls to speak to — and perhaps even soothe — incoming troops trying to cope with the same thoughts and impulses. The creations give service members a format “to say what they can’t say out loud — because it’s too painful or because we just don’t feel like anybody really wants to hear it,” said Hall, who remains on active duty, stationed at Rock Island Arsenal in northwestern Illinois. “I absolutely believe it is a method to calm your mind.”
0 Comments
REGISTER Come to Topeka, Kansas Saturday, November 7, 2015! Bring your group to the Capital City of Kansas and march in the Topeka Veteran's Parade at 11am, Staging begins at 9am! Hotel, tourism and travel packages are coming soon; join our email list (below) to receive this information as soon as it’s available!
We invite you to part of the celebration at the 2015 Topeka's Veteran's Parade as Veterans from all eras march or ride around the Kansas State Capital to be honored and celebrated! PARTICIPATION: EVERYONE IS WELCOME TO WALK, DRIVE or BE in the Topeka Veterans Parade! This year everyone is welcome to have a float, car bike or walk in the Topeka Veterans Parade. ALL Participants are requested to have a patriotic theme (red white & blue) colors on their clothing, cars, bikes or flags displayed. Registration is open now! STAGING NOTICE: Staging lanes will open at 9am for participants! STAGING ENTRANCE WILL BE AT 5TH & TOPEKA BLVD All floats, cars and participants MUST have Patriotic themes. RED, WHITE & BLUE! All vehicles, cars, trucks, jeeps must have signs acknowledging the veterans in the cars. Questions or Concerns please email contact@militaryveteranproject.org We also encourage you to connect with us on Facebook and Twitter (@Topekaveterans). Come to Topeka, Kansas! Bring your group to the Capital City of Kansas and march in the 2014 Veteran's Parade! Hotel, tourism and travel packages are coming soon; join our email list (below) to receive this information as soon as it’s available! Contribute! Sponsorship packages are available for corporations and organizations wishing to show their support for our veterans. To learn more, contact us using the form below. In addition, individuals may contribute online here. DONATE
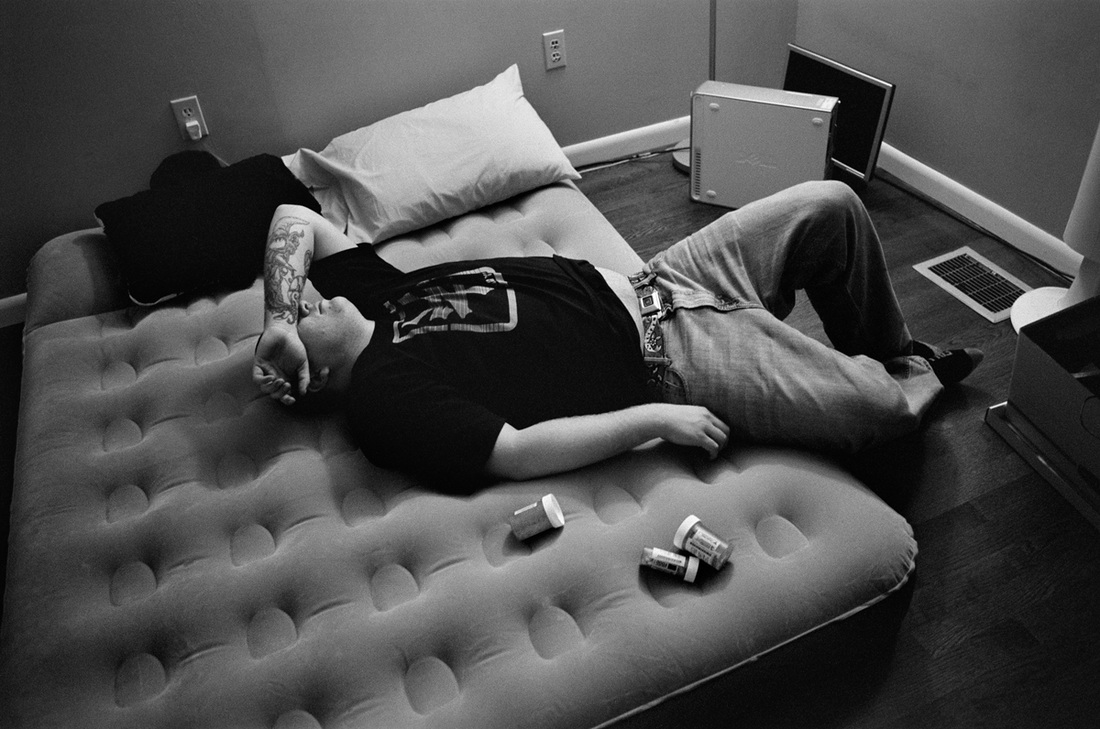
You lay awake at night and can’t sleep. You’re restless and feel tired during the day. Nightmares wake you up. You’re unable to go back to sleep. Are sleeping problems making it hard for you to get through the day? Sometimes trouble sleeping is a result of a traumatic experience or stressful event in your military or civilian life. Other times, negative thoughts or worry might make it hard to fall asleep or cause you to wake up easily during the night. Trouble falling asleep may be due to anxiety about having nightmares, or from thoughts focused on life challenges. Chronic pain, stomach problems, alcohol or drug use, or other physical ailments also might disturb your sleep. Inadequate sleep over time can lead to chronic sleep deprivation, which will significantly affect your health, performance, and safety.
Good sleep is important for overall good health. The amount of sleep each person needs varies, but seven to nine hours of sleep is ideal for most adults. To feel well rested, your body also needs to go through a series of sleep stages. When those sleep stages are interrupted, you may feel especially tired or have trouble concentrating the next day. “I used to fall asleep so easily during my deployment, even with all the loud noises and 24/7 commotion, but now that I’m back and in a quiet, comfortable bedroom, I just can’t seem to fall asleep at night.” Some Veterans don’t realize their trouble sleeping is affecting their day-to-day functioning or that their sleeping problems are treatable. Symptoms of sleep deprivation and other sleep problems include:
“I used to have a drink every night to get to sleep. One day my friend dug out a week’s worth of empty liquor bottles from the trash and put them on the table for me to see. It was right then I decided to stop self-medicating to get to sleep and address the issue once and for all.” There are several things you can do right away to improve your sleep. Try to remember to:
*Please note the Military Veteran Project does not endorse the AtEase study, merely sharing information for veterans and families to become educated on the correlation and options to participate. Currently, the Military Veteran Project is working with hundreds of veterans to treat Post Traumatic Stress with alternative therapies and treatments while conducting research for Traumatic Brain Injury. To learn more visit WHY WE EXIST - Together, we know we can make a difference and save lives. Relationships and PTSD
How does trauma affect relationships? Trauma survivors with PTSD may have trouble with their close family relationships or friendships. The symptoms of PTSD can cause problems with trust, closeness, communication, and problem solving. These problems may affect the way the survivor acts with others. In turn, the way a loved one responds to him or her affects the trauma survivor. A circular pattern can develop that may sometimes harm relationships. How might trauma survivors react?In the first weeks and months following a trauma, survivors may feel angry, detached, tense or worried in their relationships. In time, most are able to resume their prior level of closeness in relationships. Yet the 5% to 10% of survivors who develop PTSD may have lasting relationship problems. Survivors with PTSD may feel distant from others and feel numb. They may have less interest in social or sexual activities. Because survivors feel irritable, on guard, jumpy, worried, or nervous, they may not be able to relax or be intimate. They may also feel an increased need to protect their loved ones. They may come across as tense or demanding. The trauma survivor may often have trauma memories or flashbacks. He or she might go to great lengths to avoid such memories. Survivors may avoid any activity that could trigger a memory. If the survivor has trouble sleeping or has nightmares, both the survivor and partner may not be able to get enough rest. This may make sleeping together harder. Survivors often struggle with intense anger and impulses. In order to suppress angry feelings and actions, they may avoid closeness. They may push away or find fault with loved ones and friends. Also, drinking and drug problems, which can be an attempt to cope with PTSD, can destroy intimacy and friendships. Verbal or physical violence can occur. In other cases, survivors may depend too much on their partners, family members, and friends. This could also include support persons such as health care providers or therapists. Dealing with these symptoms can take up a lot of the survivor's attention. He or she may not be able to focus on the partner. It may be hard to listen carefully and make decisions together with someone else. Partners may come to feel that talking together and working as a team are not possible. How might loved ones react?Partners, friends, or family members may feel hurt, cut off, or down because the survivor has not been able to get over the trauma. Loved ones may become angry or distant toward the survivor. They may feel pressured, tense, and controlled. The survivor's symptoms can make a loved one feel like he or she is living in a war zone or in constant threat of danger. Living with someone who has PTSD can sometimes lead the partner to have some of the same feelings of having been through trauma. In sum, a person who goes through a trauma may have certain common reactions. These reactions affect the people around the survivor. Family, friends, and others then react to how the survivor is behaving. This in turn comes back to affect the person who went through the trauma. Trauma types and relationshipsCertain types of "man-made" traumas can have a more severe effect on relationships. These traumas include:
Do all trauma survivors have relationship problems?Many trauma survivors do not develop PTSD. Also, many people with PTSD do not have relationship problems. People with PTSD can create and maintain good relationships by:
If you need to seek professional help, try to find a therapist who has skills in treating PTSD as well as working with couples or families. For resources, please see our Where to Get Help for PTSD page. Many treatment approaches may be helpful for dealing with relationship issues. Options include:
This time of year we see lots of ads for red roses and romantic dinners. While those are certainly important components of romance, lasting love involves two people taking care of each other. In some marriages, that may include being alert for signs of PTSD in your spouse.
With the hustle and bustle of everyday life, it can be hard to know when your partner is struggling. In our daily interactions as couples, we sometimes misunderstand each other, tensions arise and we fight. Then, we withdraw from each other. This is a normal interaction between spouses, right? Not always. Perhaps the tension you feel is because your partner is feeling the effects of PTSD. It is not always easy to figure out if someone has PTSD, but there are some signs that can clue you in. In some cases it can be very obvious. For instance, if your service member returns from a deployment and is still having difficulty falling asleep, wakes up in a cold sweat and punches at an imaginary foe, months after he or she returns, PTSD may be the culprit. In other cases, the signs might not be as obvious. Your partner could gradually withdraw from activities and people he otherwise enjoyed. You might notice him having nightmares and difficulty falling asleep. He might feel emotionally numb and could appear anxious, worried, angry or moody. When the symptoms are milder it can be difficult to tell the difference between everyday stress and PTSD. Here’s the main difference: everyday stress doesn’t last long. Your partner may feel out of sorts, anxious and have trouble sleeping because of stress in his or her life, problems at work, or in a relationship. The stress is temporary. The stress resolves and doesn’t affect everyday life in a significant way. It also may not follow a particularly traumatic event. This is not the case with PTSD. PTSD symptoms continue for longer than the average stress episode. Signs to Watch In most cases, PTSD sets in after a traumatic event has taken place, such as the violent death of a friend or family member, combat experience, or a natural disaster. It also lasts. It doesn’t just go away, and it affects their everyday life. You may notice your partner has recurring nightmares or thoughts about a traumatic event. You may see trouble sleeping and eating, or have a marked increase in anxiety and fear. Your partner may be on edge, easily startled and overly alert. At other times he could appear depressed, with a low energy level, memory loss and a lack of focus. He may have difficulty making decisions, and avoid people, places or activities that would normally make your spouse happy. You may suddenly feel like you are walking on egg shells, afraid you might "set him off." You begin to worry that your partner is no longer himself. He may be suffering from PTSD, and it is not his fault, nor is it your fault, but he does need help. Here is a list of symptoms to look for in your spouse or partner which may indicate they have PTSD:
In this month where relationships are the focus, take an inventory of your relationship. Is your spouse experiencing any of the above symptoms? If so, contact a mental health provider in your area for an assessment, diagnosis and plan. If your spouse is actively suicidal, get help right away. And remember, you are not alone. Help is out there for you and your spouse so that you can have a happier and healthier relationship. Freemane Brown, 54, lied about military service and wore Navy uniforms, ribbons, and other awards to beg for money, according to deputies.Brown, 54, was charged with unlawful use of uniforms, medals, or insignia, which is a felony. On August 7, a citizen told Hillsborough County Sheriff's Office that a man wearing a military uniform was aggressively soliciting money for veterans at the Wawa Store at 804 E Bearss Ave in Tampa. When deputies went to check it out, they found Brown on the east side of the store wearing a United States Navy uniform with a rank of Commander and 21 ribbons to include the Navy Cross and Silver Star, along with the Navy Seal Trident and Jump Wings. Deputies observed many of the items on the military uniform were not in compliance to standard military regulations. Deputies made contact with the manager of the Wawa store and she advised she gave permission to Brown two days earlier to stand outside the store since she believed Brown was a veteran. During questioning, Brown first made statements he was a former member of Seal Team Six and traveling all over the world. After further questioning, Brown admitted he was never a Navy Officer and never served as a Navy Seal. Deputies learned Brown purchased all of his military insignias including the Navy uniform at a local Army/Navy surplus store. Deputies also noted Brown had a name tag on the uniform, but his name was covered with a small piece of black tape. Brown voluntarily surrendered all of the military insignias at the scene. On August 12, Brown was arrested at his home and booked into the Hillsborough County Jail. What is Stolen Valor?
The Stolen Valor Act of 2013 (Pub.L. 113–12; H.R. 258) is a United States federal law that was passed by the 113th United States Congress. The law amends the federal criminal code to make it a crime for a person to fraudulently claim having received any of a series of particular military decorations and awards with the intention of obtaining money, property, or other tangible benefit from convincing someone that he or she rightfully did receive that award. However wearing a military uniform in public with no prior service isn't illegal, it only becomes illegal when someone takes credit for serving in the military when no service has been done. Have you seen someone who you think may be committing stolen valor? Visit our friends at Stolen Valor / Guardian of Valor with questions or concerns.. They served our country proud and fought for our freedom, but now many are paying a price they shouldn't have to pay. One in five veterans suffers with combat-related post-traumatic Stress Disorder (PTSD) and struggles to reintegrate back into society. Help is available, but many veterans continue to needlessly suffer for a number of reasons. Many veterans go to their civilian primary care physician (PCP) than to the doctors at the VA for treatment of their PTSD symptoms. What's needed is increased education for both primary care physicians and veterans when it comes to PTSD.
Commonly experienced symptoms of military PTSD include: inappropriate anger or irritability; insomnia; problems on the job and at home; acting detached or distant; having trouble with social events such as weddings, funerals and other family gatherings; and being easily startled or hyper vigilant. Once the veteran is seen by his family doctor, a PTSD diagnosis is often missed for two reasons: First, primary care physicians simply don't have the specific training to recognize or treat combat-related PTSD. It's not uncommon for the physician to write the patient a script for an antidepressant or anti-anxiety medication and send him on his way, failing to recognize there is a deeper underlying issue. In addition, many doctors have little time to spend with patients, and therefore are simply unable to fully explore all symptoms and give adequate information about the best treatment options. Second, the patient fails to inform his doctor that he is a veteran and spent time in the combat theatre, and more than likely the physician fails to inquire. The patient's symptoms are attributed to stress or a rough patch that should hopefully improve with time. To ensure that a proper diagnosis of PTSD is not missed, better education for both veterans and primary care physicians needs to become the new standard protocol. For the veteran 1. Recognize you might have PTSD. If you spent time overseas and experienced war, violence, bloodshed and death, PTSD is a real possibility. Don't be afraid to admit you might have PTSD because of the stigma and misinformation about the condition. 2. Educate yourself on the symptoms of PTSD, and ask for input from your loved ones about their observations of your symptoms and behaviors. Learn about the condition before you go to the doctor. 3. Take a list of your symptoms (including those suggested by your loved ones) in writing to your physician. This allows for more efficient use of your time with the doctor. 4. Be open to suggestions your doctor might have for treatment of your condition. Don't be fearful of asking appropriate questions about suggested further evaluations, treatments or referrals. Remember the treatment of PTSD is not something the doctor does to you, but rather a process that you and your doctor (or therapist) engage in as a team. 5. In general, treatment for PTSD can include both talk therapy (psychotherapy) alternative therapies, as well as medication. Your doctor may want to refer you to a therapist or psychiatrist (VA or civilian) for more specialized care. Last but not least, reach out to a battle buddy or reach out to Battle in distress Finally, know that doing nothing, or hoping that time will heal PTSD, are generally ineffective ways of dealing with it. Treatment will only work if recommendations are appropriate and are followed and the veteran becomes an active and willing partner in the treatment process. For primary care physicians 1. Primary care physicians need to realize that millions of Americans served in Iraq, Afghanistan and other parts of the world. The chance a patient is a veteran is very likely, and asking "Are you a veteran?" needs to become standard practice. 2. Primary care physicians need to attend more continuing medical educations programs that teach the right questions to ask veterans, along with the signs and symptoms to look for that could point to PTSD. 3. Offer the veteran reassurance that you are not there to judge him or her, but your role is to serve as an ally in his treatment and recovery. Always be optimistic with the veteran and supportive but not enabling. Combat-related PTSD is the "silent killer" of the military because it's often misdiagnosed, and without the right help it can be extremely debilitating and is linked to an increased risk of suicide. Join the #22ADAY Movement to bring awareness in your area and help save a life by clicking here. Read more about what the Military Veteran Project is doing to treat post traumatic stress and research traumatic brain injury to help end military suicide. http://www.militaryveteranproject.org/news/brain-scans-can-tell-traumatic-brain-injury-and-post-traumatic-stress-disorder-apart |
Sign up for our mailing list by clicking here
Archives
March 2020
|
|
Get to know us
|
Resources
|
Get Involved
|
|
|
|
|
The Military Veteran Project is a non-profit 501 (c)3 organization, IRS identification number 46-0877378. Donations made to the Military Veteran Project are tax deductible in the U.S. ·







 RSS Feed
RSS Feed